One of the 12 labors of Hercules, in accordance to historic lore, was to destroy a nine-headed monster referred to as the Hydra. The problem was that when Hercules used his sword to chop off one of many monster’s heads, two would develop again in its place. He subsequently wanted an extra weapon, a torch, to vanquish his foe.
There are parallels between this legend and our three-years-and-counting battle with SARS-Cov-2, the virus that causes Covid-19. Every time scientists have thought they’d subdued one pressure of the virus — be it alpha, beta, delta, or omicron — one other variant or subvariant emerged a brief whereas later.
For this cause, researchers at MIT and different establishments are getting ready a new technique in opposition to the virus — a novel vaccine that, not like these in use at this time, might probably counteract all variants of the illness, having a property referred to as “pan-variance” that would circumvent the necessity for a totally different booster shot each time a new pressure comes into circulation. In a paper revealed at this time in the journal Frontiers in Immunology, the crew experiences on experiments with mice that exhibit the vaccine’s effectiveness in stopping demise from Covid-19 an infection.
Viral vaccines sometimes work by exposing the immune system to a small piece of the virus. That can create realized responses that shield folks later once they’re uncovered to the precise virus. The premise of ordinary Covid-19 vaccines, corresponding to these produced by Moderna and Pfizer, is to activate the a part of the immune system that releases neutralizing antibodies. They do that by offering cells with directions (in the type of mRNA molecules) for making the spike protein — a protein discovered on the floor of the Covid-19 virus whose presence can set off an immune response. “The problem with that approach is that the target keeps changing” — the spike protein itself can differ amongst totally different viral strains — “and that can make the vaccine ineffective,” says David Gifford, an MIT professor in electrical engineering and laptop science and organic engineering, in addition to a coauthor of the Frontiers paper.
He and his colleagues, accordingly, have taken a totally different method, choosing a totally different goal for his or her vaccine: activating the a part of the immune system that unleashes “killer” T cells, which assault cells contaminated with the virus. A vaccine of this type won’t maintain folks from getting Covid-19, nevertheless it might maintain them from getting very sick or dying.
A key innovation made by this group — which included researchers from MIT, the University of Texas, Boston University, Tufts University, Massachusetts General Hospital, and Acuitas Therapeutics — was to carry machine studying methods into the vaccine design course of. A important side of that course of entails figuring out which elements of SARS-Cov-2, which peptides (chains of amino acids which can be the constructing blocks of proteins), ought to go into the vaccine. That entails sifting by way of hundreds of peptides in the virus and selecting out simply 30 or in order that needs to be included.
But that call has to take into consideration so-called HLA molecules — protein fragments on the floor of cells that function “billboards,” telling immune cells (which lack X-ray imaginative and prescient) what goes on inside different cells. The show of particular protein fragments can point out, as an illustration, that a sure cell is contaminated by SARS-Cov-2 and needs to be gotten rid of.
Machine studying algorithms had been used to resolve a sophisticated set of “optimization problems,” notes Brandon Carter, a PhD scholar in MIT’s Department of Electrical Engineering and Computer Science, an affiliate of the MIT Computer Science and Artificial Intelligence Laboratory (CSAIL), and a lead creator of the brand new paper. The overriding purpose is to choose peptides which can be current, or “conserved,” in all variants of the virus. But these peptides additionally want to be related to HLA molecules which have a excessive chance of being displayed to allow them to alert the immune system. “You want this to happen in as many people as possible to get maximum population coverage from your vaccine,” Carter says. Furthermore, you need every particular person to be lined a number of occasions by the vaccine, he provides. “This means that more than one peptide in the vaccine is predicted to be displayed by some HLA in each person.” Achieving these varied aims is a job that may be considerably expedited by machine studying instruments.
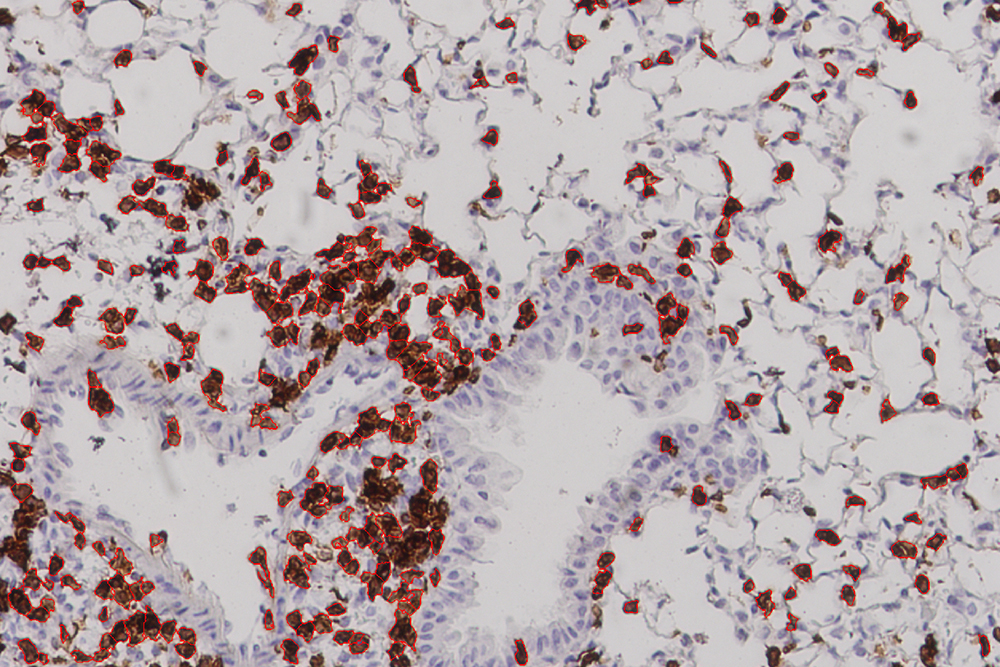
While that touches on the theoretical finish of this challenge, the newest outcomes got here from experiments carried out by collaborators on the University of Texas Medical Branch in Galveston, which confirmed a robust immune response in mice given the vaccine. The mice in this experiment didn’t die however had been had been “humanized,” that means that that they had an HLA molecule discovered in human cells. “This study,” Carter says, “offers proof in a living system, an actual mouse, that the vaccines we devised using machine learning can afford protection from the Covid virus.” Gifford characterizes their work as “the first experimental evidence that a vaccine formulated in this fashion would be effective.”
Paul Offit, a professor of pediatrics in the Division of Infectious Diseases at Children’s Hospital of Philadelphia, finds the outcomes encouraging. “Lots of people marvel about what approaches might be used to make Covid-19 vaccines in the longer term,” Offit says. “Given that T cells are important in safety in opposition to extreme Covid-19, future vaccines that focus on inducing the broadest T cell responses might be an vital step ahead in the subsequent technology of vaccines.”
More animal research — and eventual human research — would have to be completed earlier than this work can usher in the “next generation of vaccines.” The proven fact that 24 p.c of the lung cells in vaccinated mice had been T cells, Gifford says, “showed that their immune systems were poised to fight viral infection.” But one has to watch out to keep away from too robust of an immune response, he cautions, in order not to trigger lung injury.
Other questions abound. Should T-cell vaccines be used as a substitute of, or in mixture with, commonplace spike protein vaccines? While it could be doable to improve current vaccines by together with a T-cell part, Gifford says, “putting two things together may not be strictly additive, as one part of the vaccine could mask the other.”
Nevertheless, he and his colleagues imagine their T-cell vaccine has the potential to assist immunocompromised people who can not produce neutralizing antibodies and thus might not profit from conventional Covid vaccines. Their vaccine may additionally alleviate affected by “long Covid” in individuals who proceed to harbor reservoirs of the virus properly after their preliminary an infection.
The mechanism behind present flu vaccines, like present Covid-19 vaccines, is to induce neutralizing antibodies, however these vaccines don’t at all times work for various influenza strains. Carter sees potential for flu vaccines primarily based on a T-cell response, “which may prove to be more effective, providing broader coverage, because of their pan-variance.”
Nor are the strategies they’re growing restricted to Covid-19 or the flu, he maintains, as they may sometime be utilized to most cancers. Gifford agrees, saying that a T-cell vaccine — designed to maximize immune safety each inside a person and among the many best variety of people — might turn out to be a key asset in the combat in opposition to most cancers. “That’s not within the scope of our present study,” he says, “but it could be the subject of future work.”
Other MIT contributors to the work had been Ge Liu and Alexander Dimitrakakis. The work was supported, in half, by Schmidt Futures and a C3.ai Digital Transformation Institute grant to David Gifford.